- 02 9712 1736
- [email protected]
- 212 Great North Road, Five Dock, NSW 2046
- Open 7 days a week
Can stress cause a headache? Absolutely. Stress often triggers tension headaches, making you feel like there’s a tight band around your head and a constant aching pain. A tension headache is one of the most common complaints chiropractors and osteopaths manage. In this article, we’ll explore why this happens, how to recognise the symptoms and share tips to manage or prevent these headaches.

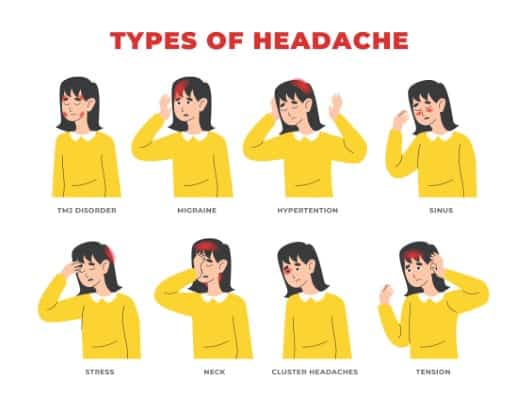
Stress-related headaches, often referred to as tension headaches, are closely linked to stress and muscle tension. These headaches are characterized by a sensation of tightness or pressure around the head, almost as if a tight band is squeezing it. They are the most common type of headache, affecting people of all ages and backgrounds.
Tension headaches are described as a dull ache that develops gradually and can affect both sides of the head. Unlike migraines, they do not usually cause nausea or sensitivity to light. Knowing the nature of these headaches aids in identifying triggers and finding effective relief methods.

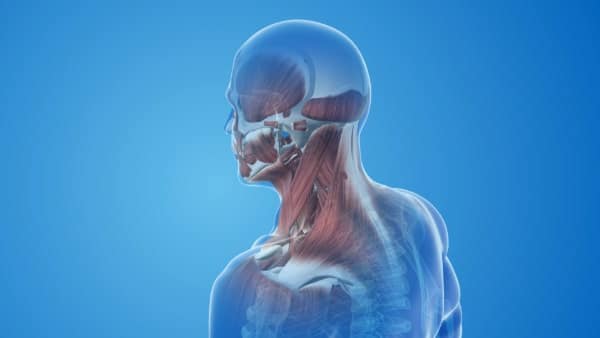
The primary cause of stress-induced headaches is emotional or physical stress, which often leads to muscle tension. When you’re stressed, your body tends to tense up, especially in areas like the scalp, neck, and shoulders. This muscle tension can lead to the development of tension headaches.
Other factors such as fatigue, overexertion, and even chronic stress can exacerbate these headaches. Recognizing these causes aids in developing strategies to manage stress and reduce headache frequency.
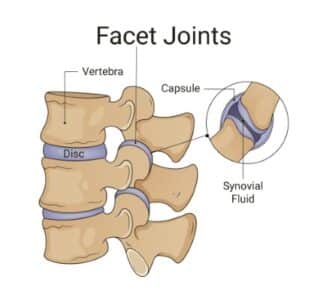
Muscle tension is a significant contributor to tension headaches. Stress can cause muscle contractions in the scalp, neck, and shoulders, leading to a headache. These muscle contractions are often the result of emotional stress or physical strain. Poor posture, such as slouching or craning the neck, can also contribute to muscle tension and trigger headaches.
Increased sensitivity to pain is another factor that might explain why some people are more prone to tension headaches than others. Recognizing these mechanisms helps identify effective treatments and preventive measures.
Hormonal changes can also play a role in stress-induced headaches. Stress triggers hormonal fluctuations in the body, which release chemical signals that can exacerbate headache pain. Awareness of this connection guides effective management strategies. This is especially true for those experiencing headaches during hormonal changes like menstruation or menopause. By managing the stress response you can experience relief of your symptoms.
Lifestyle factors, including prolonged poor posture and inadequate sleep, can significantly contribute to the development of stress-related headaches. Slouching or maintaining the same head position for extended periods can lead to muscle tension, while lack of sleep can increase stress levels, creating a vicious cycle of headache triggers. Having enough sleep is an essential factor in treating stress headaches.
Stress-related headaches can manifest in various forms, including tension headaches, migraines, and chronic headaches. Common symptoms of tension headaches include a dull ache and a tight band sensation around the head. These headaches typically develop gradually and affect both sides of the head.
Migraine headaches, on the other hand, may present with symptoms such as visual disturbances, nausea, and a unilateral intense throbbing pain. Chronic tension-type headaches can lead to persistent daily head pain and neck strain, significantly impacting daily activities and overall quality of life.
Tension headaches, the most common type, are characterized by pain in the head, scalp, or neck, often accompanied by muscle tightness. Key symptoms include a dull ache and a tight band sensation around the head, typically affecting both sides. Tension headaches occur frequently in individuals experiencing stress.
People experiencing tension headaches often report a sensation of tightness or pressure around the forehead. Muscle tenderness in the scalp, neck, and shoulder areas is also common, indicating muscle strain associated with the headache. Massage of the neck and shoulders often refers pain to where the tension headache is occurring. This is a good sign that you have a muscle-induced tension headache.
Migraines can involve visual disturbances such as seeing spots or flashes of light, which are not present in tension headaches. These headaches are often described as intense throbbing pain, usually on one side of the head. A true migraine is difficult to “push through” and people are frequently confined to bed for a period of days. Fluctuations in estrogen levels can significantly influence migraines, especially in women.
Unlike tension headaches, migraines can also cause nausea and sensitivity to light and sound, making them more debilitating for those who suffer from them.
Chronic tension-type headaches often occur daily and can last for several hours or may be constant. These headaches can significantly impact job productivity and daily activities, making it difficult to attend social or work-related commitments. Chronic headaches develop when people fail to treat the symptoms of a tension headache.
Frequent pain from chronic headaches reduces one’s ability to function normally in personal and professional environments.
Diagnosing tension headaches involves patient interviews and physical examinations by healthcare providers. There are no specific tests for diagnosing tension headaches, but other tests may be conducted to rule out other issues. Tracking headache details is vital for an accurate diagnosis, helping healthcare providers identify patterns and potential triggers for tension headaches diagnosed.
Consult a doctor if headaches disrupt daily life or worsen over time. Persistent morning headaches accompanied by nausea warrant medical evaluation to rule out more serious conditions.


The primary goal of treatment for tension headaches is to prevent tension headaches. The first step is to relieve you of your symptoms. Then it is essential to establish the underlying trigger and create change in this area of your life, to prevent the headache. Common strategies involve adopting healthy habits, changing poor posture, improving diet, utilising non-medical treatments like chiro, osteo and physio, and using appropriate medications.
Non-medical treatments, focusing on relaxation and cognitive strategies, can effectively manage stress-induced headaches. Manual therapy to relax muscle tension is the most effective form of treatment. This natural approach is also the most effective long-term strategy, as it will combine hands-on care, lifestyle modification, and health advice. Cognitive-behavioral therapy and relaxation therapy can also help reduce the frequency of tension headaches and enhance overall coping mechanisms.
Regular exercise benefits overall health and is specifically recommended to help prevent tension-type headaches. Remedial massage can help by massaging the scalp, temples, or neck, providing relief from tension headaches.
Over-the-counter (OTC) medications play a crucial role in managing pain from stress-related headaches, offering accessible relief without the need for prescriptions. Common OTC medications for tension headaches include Panadol, ibuprofen, and aspirin.
Generally effective for mild to moderate pain, these medications should be used as recommended, and individuals should consult healthcare professionals if medication overuse headaches persist.
Prescription medications are advised when over-the-counter treatments fail to manage severe or chronic headache pain. Tricyclic antidepressants are frequently prescribed as preventive medications for tension-type headaches. Preventive medicines for chronic tension headaches may take several weeks to show their full effect. It is essential you consult your general practitioner for the best approach.
Knowing the cause of your stress headache is key to any preventive strategy. Genetics, diet, and environmental triggers all contribute to stress-induced headaches. It is therefore important to consult with a healthcare professional to ensure you have established the trigger for your stress headache. The primary aim, then, of any therapy for tension-type headaches is to avert the occurrence of your headaches.
A headache diary helps doctors recognize triggers and develop effective prevention strategies.

As we have established, stress is the major contributing factor to tension headaches. This is where daily relaxation techniques are invaluable. Deep breathing and biofeedback methods are useful techniques for relaxing to manage stress and cope with tension-type headaches. Yoga and meditation have been shown to alleviate stress and reduce stress headache occurrences.
Maintaining a balanced diet rich in fruits and vegetables contributes to better stress management and headache prevention. Proper sleep hygiene and adequate hydration are also crucial to preventing dehydration-related tension headaches.
Regular sleep, exercise, and meal schedules are essential for preventing tension headaches. Poor habits such as inadequate sleep and bad posture can heighten the frequency and severity of tension headaches. Your local healthcare professional can educate you on creating a healthy lifestyle.
Another simple technique is to avoid known triggers. Being mindful to avoid triggers such as poor posture or sleep hygiene can help prevent tension headaches. A healthy, mindful lifestyle increases the likelihood of preventing stress headaches.
A headache diary helps individuals identify patterns and specific triggers for their tension headaches. Noting activities and foods consumed before a headache can provide insights into potential triggers.
Avoiding known triggers is essential for managing and preventing future headaches.

If you experience the worst severe headache ever, seek immediate medical care. Serious medical conditions that can cause headaches include a brain tumour or rupture of a weakened blood vessel (aneurysm). Urgent care is needed for sudden severe headaches or those following a head injury. If in doubt, always seek medical care.
If your headache pattern changes, see your healthcare professional.
In summary, stress-related headaches are a common and often debilitating condition that can significantly impact daily life. Understanding the causes, symptoms, and treatment options for these headaches is crucial for effective management. By adopting healthy lifestyle habits, managing stress, and recognizing headache triggers, you can reduce the frequency and severity of stress-induced headaches.
Remember, while self-care strategies can be highly effective, it’s essential to seek medical attention if your headaches persist or worsen. By taking proactive steps to manage stress and maintain a healthy lifestyle, you can reclaim your peace of mind and improve your overall well-being.
Yes, stress can indeed cause headaches, particularly tension headaches, by leading to muscle tension that exacerbates headache pain.
Tension headaches commonly present as a dull ache and a tight band sensation around the head, often accompanied by muscle tenderness in the scalp, neck, and shoulders. Recognizing these symptoms can aid in effective management.
Stress-related headaches are diagnosed through patient histories and physical examinations, along with a comprehensive tracking of headache details to identify patterns and triggers. This thorough approach allows healthcare providers to effectively determine the nature of your headaches.
For tension headaches, Panadol, ibuprofen, and aspirin can be effective over-the-counter medications for alleviating mild to moderate pain. However, consulting a healthcare professional before taking any medication is important.
You should seek medical attention for headaches if you experience the worst headache ever, notice a significant change in your headache pattern, or have sudden severe headaches, especially following a head injury. Prompt assessment is crucial in these situations.

212 Great North Road, Five Dock, NSW 2046
Onsite parking available
Phone: 02 9712 1736
Email: [email protected]
Forest Lodge, Annandale, Glebe, Leichhardt, Balmain, Haberfield, Canada Bay, Rozelle, Rodd Point, Wareemba, Stanmore, Petersham, Lilyfield, Hunters Hill, Enfield, Cabarita, Mortlake, Rhodes, Burwood Heights, Birchgrove, Gladesville, Huntleys Point, Abbotsford, Ashfield, Croydon Park, Croydon, Chiswick, Russell Lea, Burwood, Strathfield, Concord, Drummoyne, North Strathfield, Liberty Grove, Dulwich Hill, Lewisham, Camperdown, Ashbury, Homebush, Homebush West, Woolwich, Henley, Summer Hill, Sydney Olympic Park

About
Five Dock Osteopathic & Chiropractic is located in Canada Bay, in Sydney’s Inner West. Servicing suburbs including Burwood, Croydon, Drummoyne, Five Dock, Haberfield, Concord, Abbotsford, Chiswick, Leichhardt, Wareemba, Russell Lea, Summer Hill, Strathfield.
Clinic hours
Monday, Tuesday, Thursday 7AM – 7PM
Wednesday, Friday 7AM – 6PM
Saturday 7AM – 2PM
Sunday 8AM – 2PM
Contact details