- 02 9712 1736
- [email protected]
- 212 Great North Road, Five Dock, NSW 2046
- Open 7 days a week
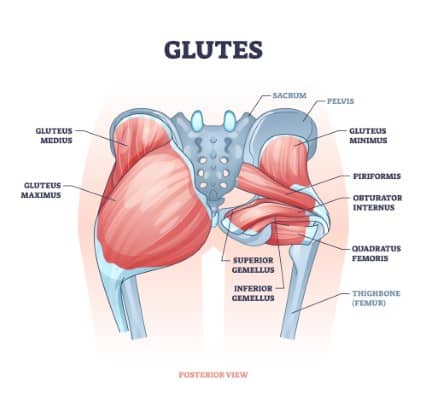
Gluteal tendinopathy is a common cause of hip pain. It affects the tendons that link the gluteal muscles to the bone. The condition causes the tendons to become inflamed and painful. Many individuals confuse this for “hip bursitis” or “greater trochanteric pain syndrome.” According to research, this illness affects as many as 14% of middle-aged women. It also affects 8% of men in the same age range.
The gluteal tendons connect your buttock muscles to your hips. They make standing, walking, and climbing stairs easier. When these tendons are damaged, you will have pain on the exterior of your hip. This soreness usually spreads down the outside of your thigh. Even simple actions like sleeping on your side become difficult. Walking upstairs or standing on one leg is also painful.
Gluteal tendinopathy, a condition that causes pain on the exterior of your hip due to inflamed tendons linking your buttock muscles, is a common issue affecting approximately 14% of middle-aged women and 8% of men. Early intervention is key to preventing the condition from worsening and improving the chances of recovery. Overuse, compression, poor movement patterns, aging, and hormonal variables all contribute to this condition. Symptoms include pain while resting on your side, walking, climbing stairs, or sitting for too long. Specific mobility tests, as well as imaging, are used to aid in diagnosis. Most people recover with conservative treatments such as load control (which reduces tendon stress), targeted exercises, and manual therapy.
Chiropractic and osteopathic treatments provide comprehensive care by integrating joint mobilisation, soft tissue massage, and exercise. Surgery is rarely required. However, it may be considered if conservative treatment fails. If you have persistent hip pain that interferes with your everyday activities, it’s crucial to seek professional help early. Make an appointment with a healthcare practitioner who specialises in musculoskeletal issues to get the right diagnosis and treatment plan.
Several factors can contribute to this painful condition. Understanding them aids in prevention and therapy.
Overuse and Repetitive Stress: Running and jumping strain these tendons. A study published in the Journal of Orthopaedic & Sports Physical Therapy validated this link. Suddenly raising exercise intensity frequently causes symptoms.
Compression: Wearing tight clothing or sleeping on your side compresses these tendons. According to research published in the British Journal of Sports Medicine, compression worsens symptoms. This explains why side sleepers frequently experience nighttime pain.
Poor Biomechanics: The way you move influences tendon health. Weak hip muscles affect the way you walk and stand. A 2018 study in Clinical Biomechanics found that suboptimal movement patterns increase tendon strain.
Ageing: Tendons normally lose strength with ageing. This makes them more susceptible to harm. After 40, tendon repair slows significantly.
Hormonal Factors: This illness affects women more than men. According to research, hormone variances may have a role in tendon difficulties. This explains the greater prevalence among middle-aged women.
Knowing the signs helps you seek treatment early. Most people with gluteal tendinopathy experience these symptoms:
Pain on the outside of the hip or buttock
Discomfort when lying on the affected side
Pain that worsens with walking or climbing stairs
Tenderness when pressing on the outside hip
Pain that gradually develops rather than suddenly
Stiffness after sitting for long periods
Difficulty with single-leg activities

Pain typically worsens with activity and improves with rest. However, sitting for too long also increases discomfort. Morning stiffness is common but usually improves after moving around.
An accurate diagnosis ensures efficient treatment. Your health care practitioner will enquire about your symptoms and activities. They will run particular tests to identify gluteal tendinopathy.
Clinical testing include leg movements that put stress on the tendons. One example is the single leg stance test, which involves standing on the injured leg. Another is the FABER test, which entails bending your knee, moving your leg outward, and rotating your foot. The word FABER stands for Flexion (bending), Abduction (moving outward), and External Rotation. According to research, these tests are capable of identifying the condition.
Imaging may be necessary in some circumstances. MRI scans provide clear evidence of tendon injury. Ultrasound can also detect inflammation surrounding tendons. A 2019 study in Skeletal Radiology indicated that these approaches were highly effective.
Research supports several treatment options for gluteal tendinopathy. Most patients improve with conservative care alone. Surgery is rarely required; however, there are specific situations where it may be considered.

Load management means carefully controlling how much stress you place on your tendons. This is the first step in healing. Research in the British Journal of Sports Medicine supports this approach. In simple terms, it means:
Temporarily avoiding activities that cause pain
Modifying how you sit, stand, and move
Avoiding positions that compress the tendons
Gradually reintroducing activities as pain decreases
A 2018 randomised controlled experiment found that load management alone reduces symptoms. After 12 weeks, patients who followed these principles experienced an 80% pain decrease.
Specific exercises help strengthen the gluteal muscles. This helps heal the injured tendons. A landmark study in the BMJ proved that exercise therapy is effective. Their research showed exercises outperformed other treatments.
Key exercises include:
Gentle gluteal muscle activation exercises
Hip abduction movements (moving leg away from midline)
Functional movement retraining
Progressive strength building
Balance and stability training
Research indicates that these activities should be performed on a regular basis. With a programme lasting 8-12 weeks producing the best results. Working with a healthcare professional ensures proper technique.

Hands-on treatments provide significant relief for many patients. This includes massage, joint mobilization, and soft tissue techniques. A 2020 study in the Journal of Manual & Manipulative Therapy confirmed these benefits.
Manual therapy helps by:
Releasing tension in surrounding muscles
Improving joint mobility in the hip and lower back
Reducing pain signals through touch-based therapies
Breaking down scar tissue around tendons
Improving blood flow to damaged tissues
Chiropractic and osteopathic care, when integrative, offers comprehensive care. Practitioners should combine massage, mobilisation and exercises for the best treatment outcomes. This integrated approach addresses all aspects of the condition. Research in the Journal of Chiropractic Medicine supports this approach. Their 2019 study showed patients improved faster with combined care.
Chiropractic and osteopatic practitioners evaluate the whole body, not just the hip. They recognise movement issues in the spine, pelvis, and legs. This whole-body approach addresses the core issues. It prevents the problem from recurring.
Treatment typically includes:
Targeted joint mobilizations and adjustments
Customized soft tissue techniques
Progressive rehabilitation exercises
Movement retraining for daily activities
Education on posture and ergonomics
A study in the International Journal of Osteopathic Medicine confirmed these benefits. Patients receiving integrated care showed 76% improvement after eight weeks.
Some people benefit from additional therapies. These alternatives can supplement primary care techniques.
Shockwave Therapy: This uses sound waves to stimulate healing. A 2020 review in the Journal of Orthopaedic Surgery and Research showed positive results. Patients experienced significant pain reduction after 3-5 treatments.
Therapeutic Ultrasound: This treatment increases blood flow to tendons. It may help some patients during early recovery. Evidence for this remains mixed.
Corticosteroid Injections: These provide short-term pain relief. However, research shows they may weaken tendons long-term. Most experts now recommend avoiding them.
Platelet-Rich Plasma (PRP): This uses your own blood components. It may promote healing in chronic cases. Research on this treatment continues to develop.
Most patients recover without the need for surgery. However, in rare cases, surgical intervention may be necessary. Surgery is typically only considered when:
Symptoms persist despite 6-12 months of proper conservative treatment
Pain severely limits daily activities and quality of life
Imaging shows significant tendon tears that won’t heal naturally
The person has failed all non-surgical approaches

Surgical options include:
Tendon Repair: The surgeon fixes tears in the gluteal tendons. This is done using small incisions and special instruments.
Tendon Debridement: This procedure removes damaged portions of the tendon. It leaves healthy tissue to heal and recover.
Tendon Release: Sometimes the surgeon cuts tight tissue around the tendon. This relieves pressure and compression on the tendon.
Recovery after surgery takes time. Most patients need 3-6 months of rehabilitation. Physical therapy is essential after surgical procedures. A 2022 study in the Journal of Hip Surgery showed 75% of patients improved after surgery.

Preventing recurrence is crucial for long-term success. Research shows these strategies help:
Maintaining hip muscle strength through regular exercise
Avoiding positions that compress the hip tendons
Using proper form during sports and exercise
Gradually increasing activity levels to avoid overuse
Wearing appropriate footwear with good support
Taking regular breaks from prolonged sitting
Using proper lifting techniques to protect your hips
A 2021 study in Physical Therapy in Sport confirmed these measures. Patients following prevention protocols had 65% fewer recurrences.
Recovery from gluteal tendinopathy takes time and patience. Research indicates that most patients experience improvement within 8-12 weeks. However, complete healing may take 3-6 months.
During the first few weeks, focus on pain management. Gradually introduce gentle exercises as symptoms improve. Around week 6-8, most people start doing more difficult strengthening. By 12 weeks, many people have returned to typical activities with modifications.
Factors affecting recovery include:
Age and overall health
How long you have symptoms before treatment
Consistency with home exercises
Addressing contributing factors like posture
Following activity modification guidelines
Schedule an appointment with a healthcare provider if you experience:
Hip pain lasting more than two weeks
Pain that disrupts sleep or daily activities
Difficulty walking or bearing weight on one leg
Pain that gets worse despite rest
Symptoms that return after initial improvement
Early intervention leads to better outcomes. Professional assessment ensures proper diagnosis. It also provides targeted treatment for your specific needs.

Gluteal tendonopathy responds favourably to the proper therapy. According to research, conservative care benefits the majority of people. Combined techniques, such as chiropractic and osteopathy, provide comprehensive treatments. These treatments address both symptoms and the underlying reasons. The key to success is persistent attention and patience. Follow your treatment plan closely. Do your specified exercises on a regular basis. Make the necessary lifestyle changes. Consult with qualified healthcare providers who understand your issue. With careful care and a gradual return to activities, most people recover completely. Understanding your illness is the first step towards healing. You can recover from gluteal tendinopathy and resume pain-free movement by following evidence-based techniques.

Forest Lodge, Annandale, Glebe, Leichhardt, Balmain, Haberfield, Canada Bay, Rozelle, Rodd Point, Wareemba, Stanmore, Petersham, Lilyfield, Hunters Hill, Enfield, Cabarita, Mortlake, Rhodes, Burwood Heights, Birchgrove, Gladesville, Huntleys Point, Abbotsford, Ashfield, Croydon Park, Croydon, Chiswick, Russell Lea, Burwood, Strathfield, Concord, Drummoyne, North Strathfield, Liberty Grove, Dulwich Hill, Lewisham, Camperdown, Ashbury, Homebush, Homebush West, Woolwich, Henley, Summer Hill, Sydney Olympic Park

About
Five Dock Osteopathic & Chiropractic is located in Canada Bay, in Sydney’s Inner West. Servicing suburbs including Burwood, Croydon, Drummoyne, Five Dock, Haberfield, Concord, Abbotsford, Chiswick, Leichhardt, Wareemba, Russell Lea, Summer Hill, Strathfield.
Clinic hours
Monday, Tuesday, Thursday 7AM – 7PM
Wednesday, Friday 7AM – 6PM
Saturday 7AM – 2PM
Sunday 8AM – 2PM
Contact details