- 02 9712 1736
- [email protected]
- 212 Great North Road, Five Dock, NSW 2046
- Open 7 days a week
The cervical spine is the upper portion of the vertebral column or your spine. It is comprised of seven vertebrae, designated C1 to C7, in the neck region. These vertebrae provide structural support, flexibility, and protection for the spinal cord, which transmits nerve signals between the brain and the body.
The structure of the spine allows for crucial movements like nodding, turning the head, and tilting. The first two vertebrae, the atlas (C1) and axis (C2), enable unique rotational movements. Neck muscles and ligaments also contribute to stability and motion. Proper care of the spine is vital to prevent injuries and maintain overall neck health.
The spinal canal is a hollow passage formed by the stacked vertebral arch and bodies in the vertebral column. The canal houses and safeguards the spinal cord, which transmits nerve signals between the brain and the body. Also within the canal surrounding the cord are protective membranes (meninges) and the cerebrospinal fluid, which provides cushioning and nourishment.
The canal’s size and shape vary along the spine, with the spinal cord’s diameter decreasing in the lower regions. Conditions like spinal stenosis, where the canal narrows, can compress the neurological structures contained within it, leading to pain and neurological issues.
The spinal cord is a crucial part of the central nervous system, running within the protective spinal canal. It is a bundle of nerve fibers and tissue that extends from the brainstem to the lower back. The cord transmits sensory and motor signals between the brain and the rest of the body, enabling movement, sensation, and reflexes. The cord is surrounded by three layers of protective membranes called meninges and bathed in cerebrospinal fluid.
Spinal cord injury and other diseases affecting the spinal cord can lead to various neurological issues, impacting mobility and sensory functions below the site of the injury.
Intervertebral discs are fibrous, cushion-like structures found between adjacent vertebrae in the spinal column. Comprising a tough outer layer (annulus fibrosus) and a gel-like center (nucleus pulposus), they act as shock absorbers and facilitate spinal flexibility. These discs provide separation, stability, and load distribution for the spine, allowing movements like bending and twisting.
With age or trauma, discs may degenerate, causing conditions like herniated discs where the gel-like material protrudes and can compress nearby nerves, resulting in pain, inflammation and discomfort. Proper posture, regular movement, and spinal care are important to maintain healthy discs.
The brachial plexus is a complex network of spinal nerves originating from the C5-T1 spinal nerve roots in the neck, which supplies the upper limbs. Multiple spinal nerve roots branch off the spinal cord and form spinal nerves near the collarbone and extends down into the arm. The brachial plexus controls movement and sensation in the shoulders, arms, and hands. It enables intricate actions like gripping and fine motor skills.
Injuries, such as stretching or compression, can affect the brachial plexus, leading to conditions like brachial plexus palsy. Rehabilitation and, in severe cases, surgical intervention may be necessary to restore function and sensation.

A herniated disc, sometimes referred to as a slipped disc, occurs when the cushion-like disc between vertebrae is damaged. This can occur in the cervical spine between cervical vertebrae or in the lumbar spine between lumbar vertebrae. As the outer layer of the disc is weakened, the inner gel-like center pushes against the outer layer resulting in a bulging disc. This results in painful symptoms such as shooting pain when the herniated disc pushes against surrounding nerve roots.
Sometimes, the outer layer of the disc becomes so damaged that the inner gel-like center is no longer contained within it. This results in a ruptured disk. The herniated disc material irritates the surrounding nerve root, causing spinal nerve inflammation and resulting in pain.
When a herniated disc occurs in the neck, symptoms may include neck pain, radiating pain down the arm and into the fingers (often along a specific nerve pathway), tingling, numbness, and muscle weakness. Pain might worsen with movements like coughing or sneezing. In severe cases, it can lead to difficulty in gripping objects or muscle weakness in the arm. Diagnosis involves imaging tests like magnetic resonance imaging (MRI) and CT scan, and treatment ranges from rest, physical therapy, and pain medication and management to surgery for more severe cases that don’t respond to conservative measures.
In the case of a lumbar disc herniation, symptoms typically involve the lower back and leg pain. Common signs include localized or radiating lower back pain, often accompanied by numbness, tingling, or weakness in one or both legs. The pain may follow a specific nerve pathway, causing sciatic pain — a sharp pain shooting down the buttocks and leg pain. Coughing, sneezing, or certain movements can intensify the pain. Muscles might feel weak or exhibit reduced reflexes. Severity of symptoms varies with some individuals experiencing mild discomfort, while others having to endure more debilitating pain. Medical evaluation and imaging tests are essential for accurate diagnosis and appropriate treatment of herniated lumbar discs.

A herniated disc typically results from disc degeneration, often due to aging and wear and tear on the spine. The discs lose water content and elasticity over time, making them more susceptible to injury, and reducing their effectiveness to act as shock absorbers. Repetitive strain, poor posture, heavy lifting, and sudden twisting motions can accelerate the process of disk degeneration.
Traumatic event like accidents or falls can also lead to disc herniation. Smoking and obesity may contribute to disc degeneration. Genetic factors can also play a role. These risk factors combined can weaken the outer layer of the disc, allowing the inner gel-like material to push through and compress nearby nerves, causing pain and related symptoms.
Several conditions with similar symptoms to a herniated disc must be considered in when making a diagnosis. Neurological signs and symptoms may be a result of compression of the nerve roots and spinal nerves as a result of something other than a herniated disk. Emergency actions should be taken in cases of severe compression with potential for long-term neurological damage. Thorough medical history, physical examination, and diagnostic tests like imaging help differentiate these conditions and guide appropriate treatment.
In the lumbar spine, it is important to rule out cauda equina syndrome, which is associated with long-term permanent neurological damage as a result of compression of the nerve root bundles called the cauda equina.
In the cervical spine, several conditions should be considered. Shoulder pain associated with cervical radiculopathy can often be caused by nerve compression due to degenerative cervical disc disease and subsequent loss of disc height and narrowing of spinal foramen where nerve exit, resulting in symptoms similar to that of a herniated disc in the neck. Other possibilities include bone spurs as a result of cervical spondylosis (degenerative changes in the spine), spinal stenosis (narrowing of the spinal canal), and myofascial pain syndrome (muscle-related pain). Inflammatory conditions like cervical arthritis or infections should also be ruled out. Rarely, conditions like tumors or vascular issues can present with similar symptoms.

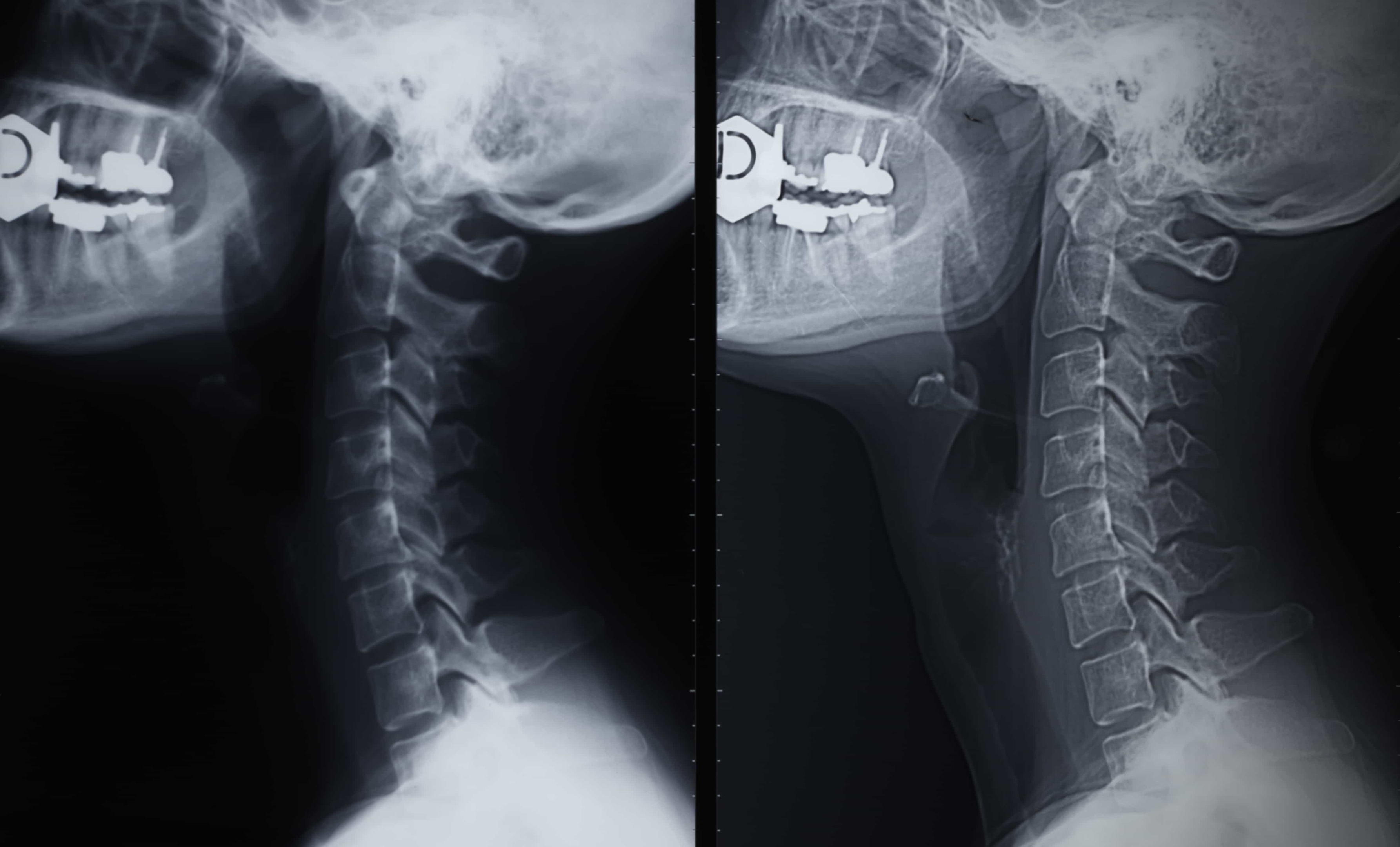
Diagnosing herniated discs involves a combination of medical history, physical and neurological examination, and diagnostic tests.A healthcare provider looks for relevant signs of symptomatic cervical disk herniation, such as neck and arm pain, numbness, and weakness if suspecting of herniated discs in the neck. They will also assess reflexes, muscle strength, and sensory function. Imaging tests like MRI or CT scan reveal the disc’s condition, its location, and its impact on surrounding structures. X-rays may show degenerative changes. Electromyography (EMG) and nerve conduction studies can identify nerve involvement and assess muscle function. Through this comprehensive approach, healthcare professionals can accurately diagnose and confirm a herniated disk and determine the best course of treatment, which may include conservative measures or, in severe cases, a referral to neurological surgeons for surgery.

Nonsurgical treatments for a herniated disk aim to relieve pain, alleviate symptoms, and promote healing. You may be referred to a physical therapist to address muscle spasms and strengthen muscles around the neck and shoulder. Physical therapy can also help improve posture and provide pain relief exercises. On your initial treatment, you will be provided with advice with regard to rest and activity modification, which plays an important role in your recovery. Physical therapy can also provide guidance with regard to lifestyle adjustments like maintaining proper ergonomics, proper lifting techniques, and regular exercise can aid recovery from disk herniation. Pain management may involve over-the-counter or prescription medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxants. Epidural steroid injection can reduce inflammation around the affected nerve. Applying ice or heat and using cervical collars might provide relief. These approaches are typically considered before surgical options are recommended for herniated disk.

Surgical treatments for a herniated disk is considered when non-surgical approaches fail to alleviate symptoms. Procedures including discectomy, artificial disc surgery, or spinal fusion may be used. One common surgical procedure is discectomy, where the herniated portion of the disc is removed to relieve nerve compression. Spinal fusion involves stabilizing the spine by fusing adjacent vertebrae together using grafts or cervical plate implants. Artificial disc surgery replaces the damaged disc with an artificial disc. Surgical approaches vary based on the severity and location of the herniation and if more than one disc is involved. These procedures aim to reduce pain, restore function, and prevent further nerve damage. Post-operative rehabilitation and follow-up care are essential for optimal recovery.
When suffering from a herniated cervical disc, it’s important to avoid activities that could worsen your symptoms or put additional strain on your neck and spine. Some activities to steer clear of include:
1. Heavy Lifting: Avoid lifting heavy objects as it can strain the neck and exacerbate disc pressure.
2. Sustained Forward Bending: Activities that involve prolonged bending forward, like gardening or vacuuming, can stress the spine and exacerbate disc pressure.
3. High-Impact Activities: Avoid activities like jumping or running that create jarring impact on the spine.
4. Poor Posture: Maintain good posture to reduce strain on the neck. Avoid slouching or hunching forward.
5. Twisting and Turning: Rapid or excessive twisting and turning motions can worsen disc issues.
6. Excessive Screen Time: Prolonged periods looking down at screens can strain the neck. Take breaks and adjust screen heights.
7. Contact Sports: Activities with a risk of impact or collision, like contact sports, should be avoided.
8. Driving Long Distances: Long periods of driving can strain the neck. Take breaks to stretch and move.
9. Carrying Heavy Bags: Carrying heavy bags on one shoulder can cause imbalances and stress on the neck.
10. High-Impact Exercise: Avoid exercises that involve heavy weights or jarring movements, especially those targeting the upper body.
Consult with a healthcare professional for personalized advice on activities to avoid based on your specific condition and symptoms.

Rehabilitation plays a crucial role in herniated disk recovery by focusing on pain relief, strengthening, and restoring function. Physical therapy includes gentle exercises that improve neck and upper body muscle strength, flexibility, and posture. These exercises help alleviate pressure on the affected disc and nerves, promoting healing. Manual therapy, such as gentle stretches and massage, can reduce muscle tension and enhance blood flow. Education about proper ergonomics and body mechanics prevents further strain. Gradual progression of exercises under professional guidance minimizes the risk of re-injury. Rehabilitation facilitates a gradual return to normal activities, enhancing overall recovery and preventing future issues.

Preventing a herniated cervical disc involves adopting healthy habits and practices to minimize the risk. Here are some preventive measures:
1. Maintain Good Posture: Sit and stand with proper posture to reduce strain on the neck and spine.
2. Use Ergonomic Equipment: Ensure that your workstation, computer setup, and chairs promote good posture.
3. Lift Correctly: When lifting, use your legs instead of your back, and avoid lifting heavy objects whenever possible.
4. Stay Active: Engage in regular physical activity to keep your neck and back muscles strong and flexible.
5. Avoid Repetitive Strain: Take breaks during repetitive tasks and incorporate stretching exercises.
6. Stay Hydrated: Drink plenty of water to keep intervertebral discs hydrated and functioning properly.
7. Maintain a Healthy Weight: Excess weight can strain the spine, increasing the risk of disc issues.
8. Use Proper Pillow: Choose a supportive pillow that aligns your neck and spine during sleep.
9. Avoid Smoking: Smoking can contribute to disc degeneration, so quitting or avoiding smoking is beneficial.
10. Stay Mindful of Movements: Avoid sudden twisting or jerking motions that strain the neck.
By incorporating these practices into your lifestyle, you can reduce the likelihood of developing a herniated cervical disc and maintain better overall neck health.


Forest Lodge, Annandale, Glebe, Leichhardt, Balmain, Haberfield, Canada Bay, Rozelle, Rodd Point, Wareemba, Stanmore, Petersham, Lilyfield, Hunters Hill, Enfield, Cabarita, Mortlake, Rhodes, Burwood Heights, Birchgrove, Gladesville, Huntleys Point, Abbotsford, Ashfield, Croydon Park, Croydon, Chiswick, Russell Lea, Burwood, Strathfield, Concord, Drummoyne, North Strathfield, Liberty Grove, Dulwich Hill, Lewisham, Camperdown, Ashbury, Homebush, Homebush West, Woolwich, Henley, Summer Hill, Sydney Olympic Park
About
Five Dock Osteopathic & Chiropractic is located in Canada Bay, in Sydney’s Inner West. Servicing suburbs including Burwood, Croydon, Drummoyne, Five Dock, Haberfield, Concord, Abbotsford, Chiswick, Leichhardt, Wareemba, Russell Lea, Summer Hill, Strathfield.
Clinic hours
Monday, Tuesday, Thursday 7AM – 7PM
Wednesday, Friday 7AM – 6PM
Saturday 7AM – 2PM
Sunday 8AM – 2PM
Contact details