- 02 9712 1736
- [email protected]
- 212 Great North Road, Five Dock, NSW 2046
- Open 7 days a week
Suffering from frequent headaches and suspect your neck might be to blame? Neck pain and stiffness can indeed trigger headaches, often leaving you searching for answers. In this article, we tackle the question ‘headaches could your neck be the cause’ head-on, discussing the anatomical connections, potential triggers, and treatment strategies, all aiming to bring you the relief you’re seeking.

Key Takeaways
Neck pain and headaches often come hand-in-hand. Tightness and stiffness in the neck and shoulder region often precedes a headache. This may be a result of poor posture, neck strain, injuries, or a combination of the above. Subsequent irritation of the cervical nerves around the neck can also result in further pain, including severe pain. Tightness in certain neck muscles can be associated quite consistently with certain types of headache presentations, highlighting the complex relationship between neck pain and headaches.
Secondary problems like increased pain sensation, visual disturbances, and dizziness may also occur as a result of neck pain-induced headaches. Headaches attributed to neck issues are typically classified as secondary headaches, distinct from primary headaches that aren’t associated with other medical conditions.


Underneath layers of skin and muscles, deep within your neck, is the cervical spine. This portion of your spine is made up of seven bones known as cervical vertebrae. These bones form the upper segment of the spine and provide structure so that the head can be lifted and held over the body. These bones are also capable of some movement relative to each other, allowing mobility so that the head can be moved. Various muscles in the neck, upper back, and shoulder work together to support the head and provide stability to the spine, while allowing for a more controlled movement of the head.
The neck also serves as a vital passageway for nerves traveling between the brain and the rest of the body, playing a key role in the central nervous system. This intricate anatomy of the neck is what makes it possible for neck conditions to impact headache experience.

Neck pain can stem from a variety of factors, including:

Other medical conditions can also result in neck pain including herniated discs and cervical radiculopathy. When nerves in the neck are irritated or compressed, you will experience symptoms such as stiffness, headaches, shoulder pain, muscle weakness, and tingling sensations. Diagnosis of neck pain depends on numerous signs and symptoms so always contact a healthcare professional if you have any of these symtpoms.
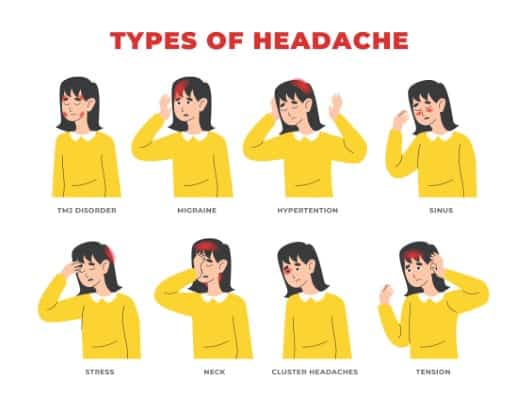
Neck pain is often associated with a few different types of headaches. Tension headaches and cervicogenic headaches, for example, are commonly associated with neck pain. Headaches that are secondary to musculoskeletal neck complaints can be chronic and vary depending on the underlying cause. A migraine headache may also be associated with a stiff neck.
Cervicogenic headaches are referred pain arising from poor mobility and function of the upper cervical spine. They are characterised by unilateral head pain and same side shoulder and arm pain. Unsurprisingly, cervicogenic headaches are often associated with reduced neck range of motion. Identifying cervicogenic headaches requires a comprehensive review of the patient’s medical history, focusing on specific criteria such as previous history, past injuries, temporal patterns, and aggravating movement and activities. It is important to establish the underlying neck dysfunction so as not to develop chronic headaches.
Physical examinations may reveal restricted cervical spine range of motion, joint dysfunction in the upper cervical spine, and significant muscle guarding in the neck. These headaches often begin as a dull ache in the neck that radiates upward, typically affecting just one side of the head.
Tension headaches are another type of headache commonly associated with neck pain and neck stiffness. Tension headaches are usually associated with mild to moderate pain. Tight muscles in the back of the neck, at the base of the skull, and over the shoulders can lead to headaches characterised as a tight band around the forehead, squeezing sensation, general head pain, and pain in the back of the neck and shoulders.
Tension headaches can be episodic, occurring less frequently but recurrent, meaning you have them often. They can also be chronic, which is more persistent and does not get better on its own. Treating a tension headache requires managing tightness in the neck and shoulders. Over-the-counter pain medications, heat, and rest can often be beneficial. If these headaches are recurrent or do not get better with time, an additional approach, such as manual therapy, may be necessary.
Occipital neuralgia is a condition that’s triggered by an injury, inflammation, or irritation of the occipital nerve, which results in burning, shooting, throbbing pain in the distribution of the occipital nerve on one or both sides of the head. Pain often starts in the neck, back of the head, and travels into the scalp, forehead, and behind the ears and eyes.
Occipital neuralgia and neck pain can present together as a consequence of occipital nerve involvement in the underlying musculoskeletal neck complaint, leading to the sharp, intense pains in the distribution of the occipital nerve.

Determining the cause of neck-related headaches involves a comprehensive diagnostic procedure that includes understanding the features of the headache, conducting a physical examination, and performing diagnostic tests. Imaging techniques such as MRI, computed tomography (CT), and/or CT myelography may be ordered to rule out certain conditions in the diagnostic process for secondary headaches.
If you’re experiencing shooting pains across the scalp or skull, it’s crucial to consult with a doctor about your symptoms and past medical history.
Diagnosing neck-related headaches requires a detailed medical history and a thorough physical examination. Physical examinations for secondary headaches typically involve assessing mobility in the cervical spine, identifying muscle tightness and imbalances in the neck, shoulder, and upper back region, and strength testing to assess for muscle weakness.
While imaging techniques can be useful, they may not reveal the underlying functional and mechanical issues resulting in these headaches, and as such may not be immediately necessary. A comprehensive physical examination has a greater value for diagnostic evaluation when determining if the headache is secondary to neck pain.
Imaging can aid in diagnosis making, offering detailed visualization of potential pain-causing structures in the neck. The choice between these imaging techniques is influenced by the specific clinical situation, as each has its strengths and limitations. The imaging techniques used for diagnosing neck-related headaches include:
To accurately diagnose the cause of neck-related headaches, radiologists and healthcare providers may refer to imaging results as part of a comprehensive evaluation, considering patient history and clinical symptoms.
Upon establishing a diagnosis, several treatment options for neck-related headaches may be utilised. These range from conservative treatments like manual therapy, medication to more invasive options such as surgical interventions.

Conservative management to relieve pain of neck-related headaches is often recommended when the condition is new or when conservative treatments have not been tried previously. Conservative management often involves physical therapy that includes prescribing exercises and stretches to strengthen neck and back muscles and improve posture and function, potentially alleviating neck-related headaches. Other treatment modalities, like massage therapy, acupuncture, dry needling, and TENS therapy, may relieve pain and contribute to the overall management of neck-related headaches.
Self-care measures such as finding an ergonomic pillow and office chair that supports the neck curvature, limiting the amount of time spent in front of the computer or on a phone, can also help manage neck-related headaches.
If conservative treatments fail to provide sufficient relief, interventional therapies may be considered. Some interventional treatments include occipital nerve blocks and corticosteroid injections. Steroid injections into cervical facet joints or the epidural space can reduce inflammation and offer temporary relief for cervical radiculopathy, potentially alleviating related headaches. Deep cervical plexus blocks temporarily numb your nerves, providing relief from pain associated with headaches. Nerve ablation may also be offered which may offer longer pain relief by destroying nerves to stop pain signals.
Should both conservative and interventional therapies prove unsuccessful to reduce pain symptoms, surgical interventions may be deemed necessary. Surgery might be required for severe cases of cervical radiculopathy if all else fails. Minimally invasive spinal cord nerve decompression surgery may be performed to treat cervicogenic headaches when they are unresponsive to other treatments. However, each case must be carefully reviewed to assess the potential benefits against the risk of complications before deciding on surgical intervention.

Although various treatment options can manage neck-related headaches, prevention remains the best strategy. Simple changes like maintaining an upright posture when sitting or standing can prevent extra weight and pressure on the head and neck, reducing the risk of pain and discomfort. Adjusting the workplace ergonomics can help prevent neck strain and consequent headaches.
Regular exercise and stretching can also help avoid headaches related to neck pain. Keeping a daily journal to note down activities and foods might unveil patterns that could identify triggers for neck pain and headaches. Sleeping with a supportive pillow to keep the head level and choosing either back or side positions can improve sleep quality to prevent neck pain and subsequent headaches.
Preventing neck strain and headaches heavily depends on workspace ergonomics. Here are some tips to help maintain a neutral head position and prevent neck pain and headaches:
To prevent neck strain while working at a computer, follow these tips:
Lifestyle modifications such as maintaining good posture, using ergonomic supports, and avoiding activities that strain the neck, can also alleviate symptoms of neck-related headaches.
Another significant factor in reducing neck pain and headaches is improving posture. Maintaining a slouched position or a forward head posture for hours creates extra stress on the muscles around your neck and your joints, potentially causing pain and contributing to headaches.
Stress or emotional factors can result in tense neck and scalp muscles, leading to the onset of tension headaches. Poor posture, particularly repeated movements and the inflammation of suboccipital muscles, contributes significantly to the development of tension headaches. By improving your posture, individuals can reduce structural imbalances and reduce stress-related tension in the neck and scalp muscles.
Preventing neck pain and headaches can be achieved with exercise and stretching. Personalized training and exercise programs that are designed to strengthen muscles, enhance flexibility, and promote body alignment can help to prevent recurrent headaches. Physical therapy methods that mobilize the joints and relieve pressure on nerves can also help alleviate pain from neck-related headaches. Regularly changing positions, standing up, and stretching hands, fingers, and arms can reduce the risk of neck pain and headaches.
Recognizing when to seek medical help for head and neck pain is essential. Persistent, intense neck pain and headaches, especially when accompanied by other symptoms, may indicate the need for medical consultation.
Further medical attention should be sought if there is uncertainty about the cause of headache and neck pain, treatments have not been effective, and there are additional worrying symptoms such as difficulty speaking, fainting spells, stiffness in the neck, or fever.

Certain symptoms and conditions require immediate medical attention. Severe neck pain occurring with a high fever could be an indication of meningitis, necessitating emergency medical care. The presence of motor difficulties, trouble walking, or severe neck pain due to a traumatic injury requires immediate emergency medical attention. Emergency care is also warranted when severe neck pain is accompanied by difficulty speaking, dizziness, fainting, and/or headache with visual disturbances, which could signal a brain tumour or mimic the signs of a stroke. Persistent or worsening cognitive symptoms like confusion, seizures, and difficulty swallowing are associated with severe underlying conditions, such as brain tumours or infections.
Should headaches persist despite treatment and preventive strategies, consulting with a healthcare professional becomes crucial. Clinicians may be concerned about headaches that increase in frequency, severity, or are accompanied by other neurological symptoms and may recommend further evaluation. Monitoring symptom progression is crucial. A headache diary can be used to help track the progression of symptoms, which is valuable information for healthcare providers.
Gradual or sudden changes in migraine headache patterns can be a warning sign. A new onset of severe headaches in an individual with no history of them, especially if over the age of 50, should prompt medical evaluation.

In summary, the intricate anatomy of the neck means that some headaches are secondary to underlying neck musculoskeletal complaints and would be preceded or accompanied by neck pain. These neck-related headaches are termed secondary headaches. Diagnosis of these headaches involves a comprehensive process including medical history, physical examination, and various diagnostic tests. A range of treatment options from conservative strategies to surgical interventions are available. However, prevention remains the best approach, and this can be achieved through posture improvement, workspace adjustments, and regular exercise and stretching. It’s crucial to seek medical help when symptoms persist, worsen, or are accompanied by other worrying symptoms.
Secondary headaches may be a result of underlying musculoskeletal neck complaints and in such cases would be preceded or accompanied by neck pain. Underlying musculoskeletal issues may be cause by triggers like poor posture, neck strain, and injuries irritating the neck nerves. Addressing underlying musculoskeletal issues will generally result in reduction of headaches.
Tension headaches and cervicogenic headaches are commonly linked to neck pain, while occipital neuralgia can also cause headaches from a pinched nerve in the neck. These conditions can be closely related to neck discomfort.
Neck-related headaches are diagnosed through a comprehensive process including a review of medical history, physical examination, and diagnostic tests such as imaging techniques.
Treatment options for neck-related headaches include conservative treatments like physical therapy or medication, and more invasive options such as surgical interventions if conservative and interventional therapies fail. Surgical interventions may be considered if symptoms persist.
To prevent neck pain and headaches, remember to maintain an upright posture, make ergonomic workspace adjustments, and incorporate regular exercise and stretching into your routine. These practices can help reduce the risk of these discomforts.
Forest Lodge, Annandale, Glebe, Leichhardt, Balmain, Haberfield, Canada Bay, Rozelle, Rodd Point, Wareemba, Stanmore, Petersham, Lilyfield, Hunters Hill, Enfield, Cabarita, Mortlake, Rhodes, Burwood Heights, Birchgrove, Gladesville, Huntleys Point, Abbotsford, Ashfield, Croydon Park, Croydon, Chiswick, Russell Lea, Burwood, Strathfield, Concord, Drummoyne, North Strathfield, Liberty Grove, Dulwich Hill, Lewisham, Camperdown, Ashbury, Homebush, Homebush West, Woolwich, Henley, Summer Hill, Sydney Olympic Park


About
Five Dock Osteopathic & Chiropractic is located in Canada Bay, in Sydney’s Inner West. Servicing suburbs including Burwood, Croydon, Drummoyne, Five Dock, Haberfield, Concord, Abbotsford, Chiswick, Leichhardt, Wareemba, Russell Lea, Summer Hill, Strathfield.
Clinic hours
Monday, Tuesday, Thursday 7AM – 7PM
Wednesday, Friday 7AM – 6PM
Saturday 7AM – 2PM
Sunday 8AM – 2PM
Contact details