- 02 9712 1736
- [email protected]
- 212 Great North Road, Five Dock, NSW 2046
- Open 7 days a week
Back pain is one of the most common health complaints worldwide. Affecting people of all ages and backgrounds. Whether it’s a dull ache after a long day or a sharp pain that limits your movement, back pain can significantly impact your quality of life. While many people experience back pain, the underlying causes can vary widely. This article explores the musculoskeletal conditions that can lead to back pain, providing a simple understanding of each.
Back pain is a complex condition that can stem from various musculoskeletal causes, ranging from common muscle strains to rare spinal disorders. While many conditions may share similar symptoms, they often require different treatment approaches. That’s why understanding the root cause of your pain is crucial for effective management. Research shows that early intervention typically leads to better outcomes, so don’t wait to seek help. If you’re experiencing persistent or severe back pain, especially if it’s accompanied by symptoms like numbness, weakness, or changes in bowel or bladder function, consult a healthcare professional for proper diagnosis and treatment.
Muscle strains occur when muscle fibres stretch too far or tear. This is often due to sudden movements, lifting heavy objects, or poor posture. The muscles in your back work constantly to support your spine and facilitate movement, making them vulnerable to injury. When strained, these muscles can become painful, stiff, and sometimes inflamed, leading to localized back pain that typically worsens with movement. Studies suggest that muscle strains account for up to 70% of low back pain cases, with a lifetime prevalence of 60-80% in the general population (Deyo & Weinstein, New England Journal of Medicine, 2001).

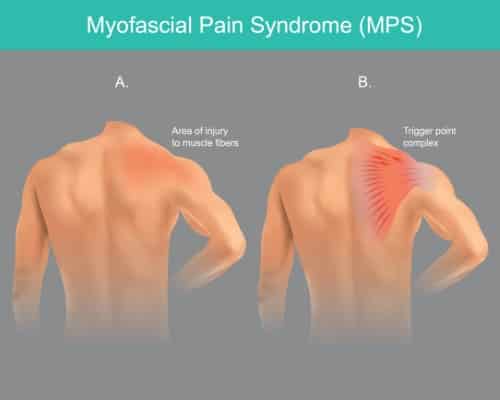
This chronic condition involves trigger points—sensitive, tight areas within muscles that cause pain when pressed. Myofascial pain often develops in the back after repetitive muscle stress or injury. The pain typically manifests as a deep, aching sensation that can radiate to other parts of the body. Unlike simple muscle strains, myofascial pain tends to persist and may be accompanied by a reduced range of motion. Research indicates that myofascial pain syndrome affects approximately 44% of people with chronic lower back pain, with a higher prevalence in women than men (Gerwin, Journal of Pain, 2005).
Our bodies function optimally when opposing muscle groups maintain a proper balance of strength and flexibility. When specific muscles become too tight or weak—often due to poor posture, repetitive movements, or a sedentary lifestyle—they can pull the spine out of its natural alignment, resulting in back pain. Common imbalances include tight chest muscles with weak upper back muscles or tight hip flexors with weak abdominals and gluteal muscles. Studies show that core muscle weakness is present in up to 80% of people with chronic low back pain (Hodges & Richardson, Archives of Physical Medicine and Rehabilitation, 1996).

Fibromyalgia is a complex condition characterized by widespread musculoskeletal pain, fatigue, and tender points throughout the body, including the back. Fibromyalgia commonly manifests with significant discomfort in the back; however, it is not exclusively a condition affecting the back. In the back, the pain is believed to result from how the brain processes abnormal pain within the central nervous system rather than from tissue or muscle damage.
Fibromyalgia pain is typically described as a constant dull ache and is commonly accompanied by sleep disturbances and mood issues. Fibromyalgia affects approximately 2-4% of the general population, with a female-to-male ratio of about 7:1, and back pain is reported by over 70% of patients (Clauw, JAMA, 2014).

Between each vertebra in your spine sits a cushion-like disc with a rigid outer ring and a soft gel-like centre. When the outer ring weakens or tears, the inner gel can bulge outward (bulging disc) or push through ultimately breaking through the outer ring (herniated disc). These conditions can irritate nearby nerves, causing pain that may radiate down the arms (if in the neck) or legs (if in the lower back). Herniated discs often cause sharp, shooting pain that worsens with specific movements. MRI studies have shown that disc herniations are present in approximately 20-36% of individuals without back pain symptoms, while clinically significant herniations account for about 4% of low back pain cases (Jensen et al., New England Journal of Medicine, 1994).
This condition refers to the natural wear and tear of spinal discs that occurs with aging. As discs lose hydration and elasticity over time, they become thinner and less effective as shock absorbers. This degeneration can lead to stiffness, reduced mobility, and pain that typically worsens with sitting or bending and improves with gentle movement. Despite its name, degenerative disc disease is actually a natural process rather than a disease. Studies show that by age 60, over 90% of individuals show some degree of disc degeneration on imaging, though only 20-25% of those with degenerative changes experience significant pain (Cheung et al., Spine Journal, 2009).
The facet joints connect the vertebrae and allow for spine movement while providing stability. When these joints become inflamed or damaged—often due to arthritis, injury, or poor posture—they can cause localized back pain. Facet joint dysfunction typically causes pain that worsens with extension (bending backward) and improves with flexion (bending forward). Research suggests that facet joint dysfunction is responsible for approximately 15-45% of chronic low back pain cases, with prevalence increasing with age (Manchikanti et al., Pain Physician, 2004).

Similar to other joint sprains, facet joint sprains occur when the ligaments supporting these joints stretch beyond their normal range or tear. This type of injury typically happens during sudden twisting or extending movements. The resulting pain is often sharp, localized to the affected joint, and worsens with specific movements, particularly extension or rotation of the spine. While specific prevalence data for facet joint sprains is limited, studies indicate that approximately 40% of acute low back pain cases involve some form of joint or ligament sprain in the spinal region (Hooten & Cohen, Mayo Clinic Proceedings, 2015).

Also known as spinal arthritis, this degenerative joint disease causes the cartilage in the facet joints to break down. As protective cartilage wears away, bone-on-bone contact can occur, leading to pain, inflammation, and the formation of bone spurs. Spinal osteoarthritis typically causes pain and stiffness that’s worse in the morning or after periods of inactivity and improves with movement. Radiographic evidence of spinal osteoarthritis is present in up to 85% of individuals over age 60, though only 30-50% of those with radiographic changes report significant symptoms (Suri et al., Osteoarthritis and Cartilage, 2012).

Ankylosing spondylitis is a type of inflammatory arthritis that primarily affects the spine, causing inflammation of the spinal joints that can lead to severe, chronic pain and discomfort. In advanced cases, inflammation can lead to new bone formation on the spine, causing sections of the spine to fuse in a fixed, immobile position. Early symptoms typically include pain and stiffness in the lower back and hips, especially in the morning or after periods of inactivity. The prevalence of ankylosing spondylitis is estimated at 0.1-1.4% globally, with onset typically occurring between ages 15-45, and men are affected 2-3 times more frequently than women (Sieper et al., Lancet, 2007).

Spinal stenosis involves the narrowing of spaces within the spine, which can put pressure on the nerves travelling through it. This narrowing most commonly occurs in the lower back and neck. Symptoms include pain, numbness, or weakness in the back, legs, neck, or arms, depending on which part of the spine is affected. The pain often worsens with standing or walking and improves with sitting or leaning forward. The prevalence of lumbar spinal stenosis is estimated at 11-38% in individuals over 60 years, making it one of the most common reasons for spine surgery in older adults (Kalichman et al., Spine Journal, 2009).
Fractures of the vertebrae can occur due to trauma, osteoporosis (compression fractures), or high-stress activities. Traumatic fractures often result from car accidents, falls, or sports injuries and can cause immediate, severe pain. Compression fractures, more common in people with osteoporosis, may cause sudden pain during an activity as simple as bending over, or develop gradually with minimal symptoms initially. Vertebral compression fractures affect approximately 25% of postmenopausal women and over 40% of women by age 80, making them the most common type of osteoporotic fracture (Cooper et al., Journal of Bone and Mineral Research, 1992).
This condition occurs when one vertebra slips forward over the one below it, often at the base of the spine. The slippage can vary from mild to severe and may be caused by a defect present at birth, trauma, or degenerative changes. Spondylolisthesis can cause lower back pain that radiates to the buttocks and legs, muscle tightness, and, in some cases, numbness or weakness if nerves are compressed. The prevalence of spondylolisthesis is approximately 4-6% in the adult population, with degenerative spondylolisthesis being more common in women over 50 (Kalichman et al., European Spine Journal, 2009).

Scoliosis is a sideways curvature of the spine that most often develops during the growth spurt just before puberty, though it can occur at any age. While mild scoliosis may not cause pain, more severe curves can lead to back pain, particularly in adulthood. Other spinal deformities, such as a kyphosis (excessive outward curvature causing a rounded upper back) or a lordosis (excessive inward curvature of the lower back causing a sway back), can also contribute to back pain by altering the spine’s natural alignment and placing additional stress on muscles and joints. The prevalence of adolescent idiopathic scoliosis (curves >10°) is approximately 2-3% of the population, while adult degenerative scoliosis affects up to 68% of individuals over age 60, with pain reported in 40-60% of cases (Schwab et al., spine, 2005).

The thoracolumbar fascia is a sheet of connective tissue that spans your lower back, connecting various muscles and the lumbar spine. When this fascia becomes tight, inflamed, or damaged, it can lead to restricted movement and pain in the lower back. This dysfunction is often associated with poor posture, repetitive movements, or inadequate core stability, and typically causes a deep, achy pain that may worsen with movement. While specific prevalence data is limited, studies suggest that thoracolumbar fascia dysfunction may be involved in 30-35% of chronic non-specific low back pain cases (Langevin et al., BMC Musculoskeletal Disorders, 2011).

The sacroiliac joints connect your pelvis to the lowest part of your spine. Dysfunction occurs when these joints move too much or too little, creating uneven movement. This can cause lower back pain that may radiate to the buttocks, groin, or back of the thigh. The pain often worsens with standing, walking, climbing stairs, or moving from sitting to standing. Research suggests that sacroiliac joint dysfunction is responsible for 15-30% of chronic lower back pain cases, with a higher prevalence in pregnant women due to hormonal changes affecting joint stability (Vleeming et al., European Spine Journal, 2012).

The iliolumbar ligaments connect the pelvis to the lower spine, providing stability to the lumbosacral junction. An iliolumbar ligament sprain can occur when these ligaments are overstretched or torn—often due to sudden twisting movements, heavy lifting, or falls. This condition typically causes sharp, localized pain in the lower back that may radiate to the hip or groin. The pain usually worsens with movement, particularly bending, twisting, or extending the back. Ligamentous injuries, including iliolumbar ligament sprains, are estimated to account for approximately 10-15% of acute low back pain presentations in primary care settings (Pool-Goudzwaard et al., Clinical Biomechanics, 2003).

The piriformis is a small muscle deep in the buttock that helps rotate the hip and the leg outward. When this muscle becomes tight or inflamed, it can press on the sciatic nerve, causing buttock pain that may radiate down the back of the leg. This condition is known as piriformis syndrome and is often triggered by prolonged sitting, stair climbing, or intense exercise involving the legs. Piriformis syndrome is estimated to account for 6-8% of patients presenting with low back pain and may be responsible for up to 17% of sciatica cases (Boyajian-O’Neill et al., Journal of the American Osteopathic Association, 2008).

Rather than a specific condition, sciatica is a symptom characterized by pain that radiates along the path of the sciatic nerve—from the lower back through the hips and buttocks and down each leg. This radiating pain occurs when the sciatic nerve is compressed or irritated, often due to a herniated disc, bone spur, or narrowing of the spine (stenosis). Sciatic pain is typically described as a sharp, electric, or burning sensation and may be accompanied by numbness, tingling, or muscle weakness in the affected leg. The lifetime incidence of sciatica is estimated at 13-40%, with an annual prevalence of 1.6-4.8%. It is most common in the 45-64 age group and affects men slightly more often than women (Konstantinou & Dunn, BMC Musculoskeletal Disorders, 2008).
Emotional stress can manifest physically in the form of muscle tension, particularly in the neck, shoulders, and back. Many people unconsciously tense their muscles when stressed, leading to chronic muscle tightness, reduced blood flow, and, eventually, pain. This stress-induced tension commonly affects the trapezius muscles (running from neck to shoulders) and the muscles along the spine, causing a dull, achy sensation that may worsen during periods of high stress. Research suggests that psychological stress contributes to approximately 30% of low back pain cases, with those reporting high-stress levels being 2.7 times more likely to experience back pain than those with low stress (Linton, Occupational Medicine, 2000).
During pregnancy, the growing uterus shifts the centre of gravity and stretches the abdominal muscles, altering posture and putting strain on the back. Additionally, as you progress through your pregnancy, hormonal changes loosen the ligaments in the pelvis. Potentially contributing to sacroiliac joint dysfunction. These factors commonly lead to lower back pain, especially in the later stages of pregnancy. The pain may range from mild discomfort to more severe pain that interferes with daily activities and sleep. Studies indicate that 50-80% of pregnant women experience back pain during pregnancy, with the prevalence increasing in the third trimester. Approximately 50-75% of women report that back pain significantly affects their daily activities (Wang et al., spine, 2004).


Though rare, tumours can develop in or near the spine, either originating there (primary tumours) or spreading from cancer elsewhere in the body (metastatic tumours). These growths can compress the spinal cord or nerves, causing back pain that may be persistent, worse at night, or unrelated to activity. Other potential symptoms include numbness, weakness, or difficulty walking. Spinal tumours require immediate medical attention, as early diagnosis and treatment are crucial. Primary spinal tumours are rare, with an incidence of approximately 2.5 per 100,000 people annually. Metastatic spinal tumours are more common, occurring in 30-70% of patients with cancer, with back pain being the presenting symptom in 90% of cases (Sciubba et al., Lancet Oncology, 2010).
DISH is a condition characterized by abnormal hardening of tendons and ligaments along the spine and other areas. This hardening leads to the formation of bone spurs that can bridge across vertebrae, restricting movement and causing stiffness and pain. DISH most commonly affects the upper and middle back and is more prevalent in older adults, particularly those with type 2 diabetes or obesity. Symptoms typically develop gradually and may include stiffness, mild to moderate pain. This is often accompanied by a reduced range of motion in the affected area.
Infections affecting the spine, such as osteomyelitis (bone infection) or discitis (disc inflammation due to infection), are uncommon but serious causes of back pain. These infections can result from bacteria entering the bloodstream and travelling to the spine.

This rare but serious condition occurs when the bundle of nerves at the end of the spinal cord (cauda equina) becomes compressed. It most commonly results from a severely herniated disc but can also be caused by tumours or infections. Symptoms include severe lower back pain, loss of bladder or bowel control, numbness in the “saddle area” (around the genitals and buttocks), and leg weakness or numbness. Cauda equina syndrome is a medical emergency requiring immediate surgical intervention to prevent permanent nerve damage.
Back pain can arise from many different origins, in the human body. These can include common muscle strains, right through to rare spinal disorders. Recognising the possible causes is the first step for effective management and treatment. While this article provides a simplified overview of many possible causes, it’s important to remember that accurate diagnosis requires professional medical evaluation.
If you’re experiencing persistent, severe, or worsening back pain—especially if accompanied by other symptoms like numbness, weakness, or changes in bowel or bladder function—consult with a healthcare provider. They can help identify the specific cause of your pain and recommend appropriate treatment options, which may include physical therapy, medication, lifestyle modifications, or in some cases, surgical intervention.
Remember that early intervention often leads to better outcomes, so don’t hesitate to seek professional advice concerning back pain.

Forest Lodge, Annandale, Glebe, Leichhardt, Balmain, Haberfield, Canada Bay, Rozelle, Rodd Point, Wareemba, Stanmore, Petersham, Lilyfield, Hunters Hill, Enfield, Cabarita, Mortlake, Rhodes, Burwood Heights, Birchgrove, Gladesville, Huntleys Point, Abbotsford, Ashfield, Croydon Park, Croydon, Chiswick, Russell Lea, Burwood, Strathfield, Concord, Drummoyne, North Strathfield, Liberty Grove, Dulwich Hill, Lewisham, Camperdown, Ashbury, Homebush, Homebush West, Woolwich, Henley, Summer Hill, Sydney Olympic Park

About
Five Dock Osteopathic & Chiropractic is located in Canada Bay, in Sydney’s Inner West. Servicing suburbs including Burwood, Croydon, Drummoyne, Five Dock, Haberfield, Concord, Abbotsford, Chiswick, Leichhardt, Wareemba, Russell Lea, Summer Hill, Strathfield.
Clinic hours
Monday, Tuesday, Thursday 7AM – 7PM
Wednesday, Friday 7AM – 6PM
Saturday 7AM – 2PM
Sunday 8AM – 2PM
Contact details